Dr. JC Suri talks about, Complete awareness on what type of Sleep Test is better for you?
A common disorder called sleep apnea makes it such that you shortly stop breathing while you sleep. Long-term, it may have serious health consequences if untreated.
You will probably go through an overnight sleep apnea test that tracks your breathing if your doctor suspects that you may have sleep apnea.
Typically, sleep studies are conducted between the hours of 10 p.m. and 6 a.m. If you’re a morning or evening person, this time period might not be ideal for you. Instead, a home test can be suggested.
You’ll spend the night in a separate room, equipped in a manner reminiscent of a hotel room with your comfort in mind. Bring your usual nighttime items, such as pajamas.
Sleep Apnea Test is used for?
To identify sleep disorders, a sleep test is used. Typical sleep problems include:
Sleep apnea is a medical disease that causes brief breathing pauses while you’re asleep. Throughout a single night of sleep, you can experience multiple recurring instances of breathing disruptions. As many as 30 episodes can be there per hour.
You may have trouble falling asleep and/or staying asleep all through the night if you have insomnia.
Restless leg syndrome makes your legs feel uncomfortable and causes a strong need to move them when you’re trying to fall asleep.
An illness of the nervous system called narcolepsy. It causes tiredness during the day. Additionally, you can suddenly find yourself napping all day.
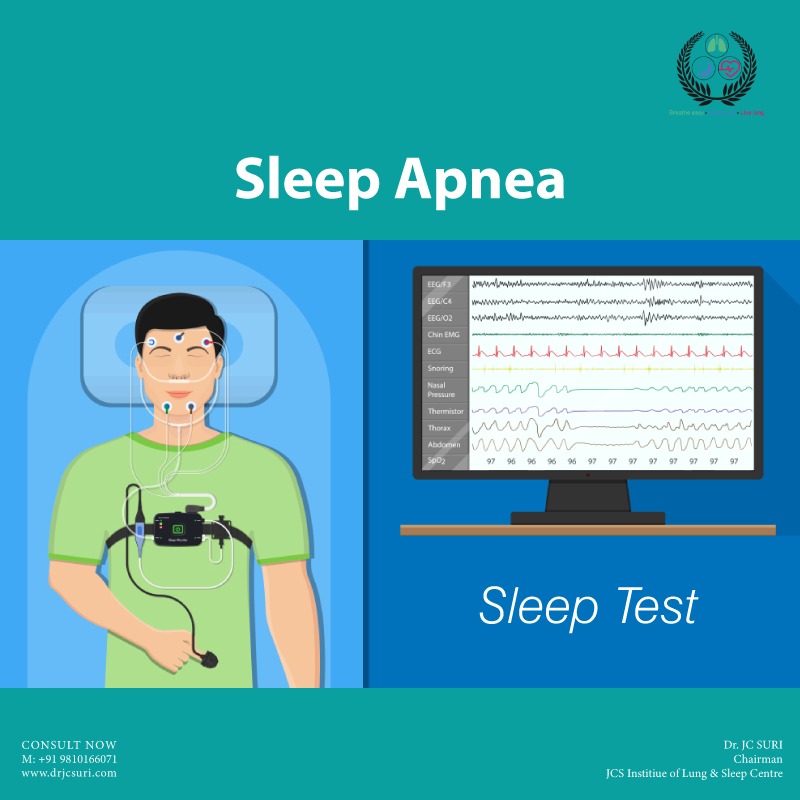
Studies on sleep are non-invasive. The donation of a blood sample is not required. But your body will be fitted with a number of wires. This makes it possible for the sleep specialist to keep an eye on your breathing, mental activity, and other vital indications while you’re sleeping.
The more at ease you are, the more accurately the technician can monitor your sleep.
After you nod off, the technician will keep an eye on the following:
- Your brain waves and eye movements, which reveal your sleep pattern
- Your blood pressure and heart rate
- Your breathing, including snoring, breathing pauses, and oxygen levels
- Your posture and any motions of your limbs
- For sleep research, there are two formats: whole night and split night.
If you take part in a full-night sleep study, your sleep will be monitored all through the night. If sleep apnea is diagnosed, you might need to return to the lab later to set up a breathing machine.
The first half of the night is utilized to track your sleep during a split-night research. In the event that sleep apnea is identified, the treatment device is set up during the second half of the night.
Pros and cons of in-lab sleep study:
In-lab sleep tests have advantages and disadvantages. Talk to your doctor about your test and preference.
Pros
Best test currently in use- The most accurate method of diagnosing sleep apnea is an in-lab sleep test.
Possibility of studying two nights in a row- Split-night studies, as opposed to full-night and at-home tests, enable diagnosis and treatment in a single night.
Best test for a particular kind of work- To achieve an accurate diagnosis, people who pose a major risk to themselves or others if they fall asleep at work should take part in an in-lab sleep study. This includes pilots, police officers, and anyone who drive for taxis, buses, or ride-sharing services.
Best choice for those who suffer from various issues or sleep disorders. People with additional medical issues, such as sleep difficulties and heart and lung ailments, are more suited for in-lab monitoring.
Cons
Costlier than an at-home test- Although not all insurance companies cover this test, if you have insurance, your insurer might pay all or part of the expense. Before you may take an in-lab exam, some providers demand the results of an at-home test..
Less accessible. In-lab research necessitates travel to and from a sleep lab. This can take a long time or cost a lot depending on where you reside.
Longer wait times. You could have to wait several weeks or even months to take the test, depending on where you reside and the demand for this kind of test.
Less convenient. It’s more likely that taking an in-lab sleep test will interfere with your everyday activities and obligations or interfere with your work schedule.
Set sleep study hours. Between the hours of 10 p.m. and 6 a.m., many sleep studies are conducted. An at-home test might be preferable if you have a diverse sleep schedule.
At-home sleep test
The motions, posture, and sleep cycles that are monitored during an in-lab exam are not monitored during an at-home test.
You can go to bed at your usual time the night of the test. To ensure that you correctly connect the monitoring sensors, pay close attention to the kit’s instructions.
Most in-home sleep apnea monitors are straightforward to set up. Typically, they consist of the following elements:
- A finger clip that gauges your heart rate and blood oxygen levels.
- A nasal cannula to gauge airflow and oxygen levels.
- Sensors that monitor your chest’s rise and fall.
- An at-home test does not track your movements, position, or sleep cycles the way an in-lab test does.
Your doctor will receive the test findings after you complete it. If therapy is required, they will get in touch with you to discuss the findings and decide on it.
Pros and Cons of a sleep test at home
Sleep tests performed at home offer benefits and drawbacks. You should discuss your preferred test with your doctor.
Pros
More convenient- Home testing is more practical than laboratory tests. You can continue with your regular bedtime routine, which may give a more accurate indication of how you breathe while you sleep than in-lab testing.
Less costly- The cost of testing taken at home is about lower.
More accessible- For those who reside a great distance from a sleep centre, at-home tests might be a more practical choice. The monitor can even be mailed to you if necessary.
Faster results- As soon as you receive the portable breathing monitor, you can start the test. Compared to a lab test, this might yield quicker results.
Cons
Less accurate- Test errors are more likely to occur in the absence of a technician. All cases of sleep apnea cannot be reliably detected by at-home tests. If you have a high-risk profession or another medical condition, this could be dangerous.
May lead to an in-lab sleep study- Regardless of the outcome of your test, your doctor can still advise an in-lab sleep test. Additionally, you might still need to spend the night in the lab to have a treatment device fitted if you are diagnosed with sleep apnea.
Doesn’t test for other sleep problems- Only breathing, heart rate, and oxygen levels are assessed during at-home examinations. This test is unable to identify narcolepsy or other prevalent sleep disorders.
Test results
The outcomes of your in-lab or at-home sleep apnea test will be interpreted by a physician or sleep specialist.
The Apnea Hypopnea Index (AHI) is a scale that physicians use to identify sleep apnea. This scale contains a calculation of the number of apneas, or breath pauses, per hour of study-related sleep.
Less than five apneas per hour are typical in those without sleep apnea or with a moderate version of the condition. More than 30 sleep apneas per hour are possible in those with severe sleep apnea.
When determining whether you have sleep apnea, doctors also check your oxygen levels. Although there isn’t a set threshold for sleep apnea, if your blood oxygen levels are lower than normal, it could be an indication.
Your doctor might advise repeating the test if the results are uncertain. Your doctor might suggest an additional test if sleep apnea is not identified but your symptoms persist.
Treatment options
Your level of sleep apnea will determine your course of treatment. Sometimes all that is needed is a change in lifestyle. These may consist of:
- Losing weight
- Using a specific pillow for sleep apnea
- Changing the location of your bed
Continuous positive airway pressure (CPAP)- There are numerous efficient medical sleep apnea therapy alternatives. Among them are: Constant positive airway pressure (CPAP). The CPAP machine is the most widely used and efficient treatment for sleep apnea. With this tool, your airways are inflated with the aid of a little mask.
Oral devices- Your throat may not close when you breathe if you have a dental appliance that moves your lower jaw forward. In cases of mild to moderate sleep apnea, these may be helpful.
Nasal device- Some people with mild to severe sleep apnea have been demonstrated to benefit from Provent Sleep Apnea Therapy, a tiny bandage-like device. It is positioned right inside the nostrils and exerts pressure to maintain your airways’ openness.
Oxygen delivery- To raise blood oxygen levels, oxygen may occasionally be provided in addition to a CPAP machine.
Surgery- When conventional therapies fail to work, surgery may be a possibility to change the way your airways are built. There are numerous surgical procedures available to treat sleep apnea.
Vital functions, such as breathing patterns, pulse rate, and oxygen levels, are measured during both in-lab and at-home sleep apnea examinations. Your doctor can diagnose sleep apnea for you using the results of these tests.
The most precise test to identify sleep apnea is a polysomnography (PSG) performed in a lab. The accuracy of tests for sleep apnea done at home is adequate. Additionally, they are more practical and economical.
Note: Do not consider JC SURI Blogs as medical advice. Never delay or disregard seeking professional medical advice from your doctor or other qualified healthcare providers because of something you have read on JC Suri.
You should always speak with your doctor before you start, stop, or change any prescribed part of your care plan or treatment. If you think you may have a medical emergency, call your doctor immediately.